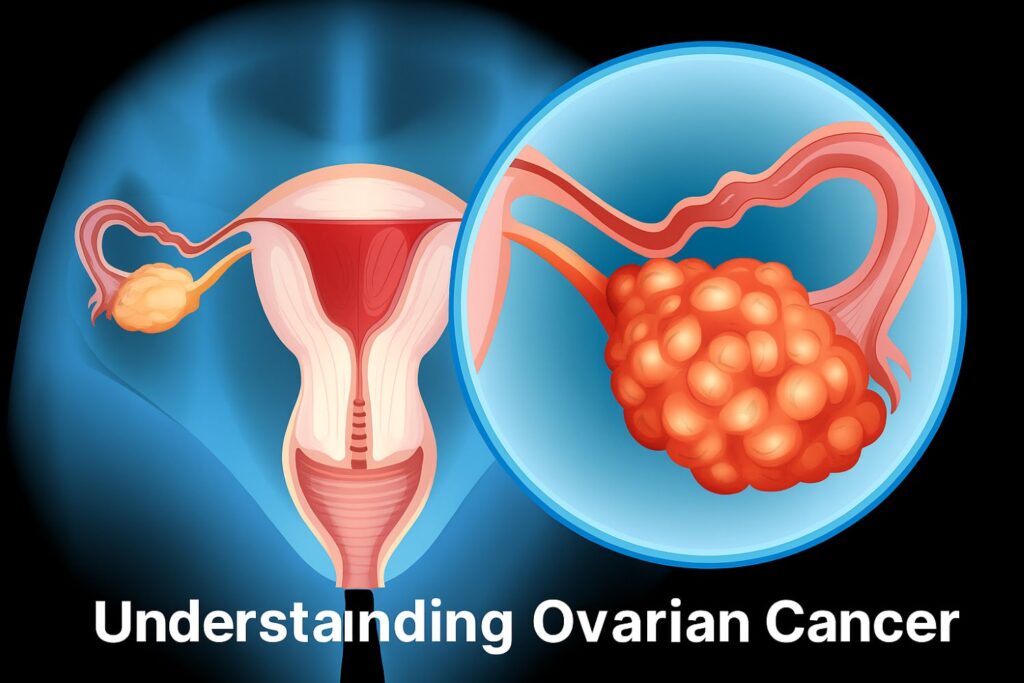
Overview & Global Impact of Ovarian Cancer
Ovarian cancer ranks among the most dangerous gynaecologic malignancies globally. Approximately 314,000 new cases and 207,000 deaths occur each year worldwide1.It is the 7th most common cancer in women and the 8th leading cause of cancer death among women globally2. Despite stable or declining age-standardized incidence in high-income countries, low- and middle-income regions are seeing rising trends2.
Why Ovarian Cancer is So Deadly
One of the critical challenges is its silent progression—symptoms at early stages are vague or absent, leading to diagnosis often at advanced stages (III/IV), when survival rates are much lower3.
Key Risk Factors for Ovarian Cancer
Non-Genetic Factors4
A comprehensive umbrella review found six non-genetic factors with strong evidence:
- Greater height: Every 10 cm increase correlates with a 16% higher risk (RR 1.16; 95% CI 1.11–1.20).
- Obesity (BMI ≥30 kg/m²): ~27% higher risk (RR 1.27; 95% CI 1.17–1.38).
- Hormone Replacement Therapy (HRT): Specific HRT regimens are associated with elevated risk.
- Oral contraceptive use: Offers protection—about a 26% reduced risk (RR 0.74; 95% CI 0.69–0.80.
Additional lifestyle and metabolic risks include:
- Obesity and diabetes mellitus—linked to both higher incidence and worse outcomes, likely due to adipokine imbalances, insulin resistance, and chronic inflammation5.
- Reproductive treatments (e.g., IVF/FT)—associated with a modest but statistically significant increased risk (OR 1.21; 95% CI 1.00–1.45 for ovarian cancer; OR 1.65; 95% CI 1.07–2.54 specifically for IVF)6.
- Environmental, genetic, and nutritional factors:
- Genetic polymorphisms such as MTHFR C677T, BSML rs1544410, and Fokl rs2228570 show small but significant risk increases7.
- Higher consumption of coffee, dietary fat, or eggs may elevate risk.
- Smoking, PCOS, endometriosis, and talc use also appear associated with increased risk; conversely, breastfeeding shows a protective effect (OR 0.72; 95% CI 0.68–0.76)8.
Genetic & Family History
While not detailed in non-genetic reviews, familial and genetic predispositions—particularly BRCA1/2 mutations—are well-established and also noted in epidemiological analyses3.
Prevention & Screening Strategies
Current Screening Limitations
To date, no screening program has proven to reduce mortality in average-risk women, despite some methods detecting cancers earlier 1. For high-risk women, surveillance every 3–4 months may downstage detection but has not yet been shown to improve survival 1.
Risk-Reducing Surgical Options
- Risk-Reducing Salpingo-Oophorectomy (RRSO) is recommended for women with lifetime risk > 4–5%. It lowers both incidence and mortality. In premenopausal women, HRT until ~51 years is advised to mitigate early menopause effects1.
- Research is ongoing into opportunistic salpingectomy, which may lower risk with fewer side effects; RRESDO (early salpingectomy with delayed oophorectomy) shows promise but remains under clinical investigation.1
References :
- Sideris M, Menon U, Manchanda R. Screening and prevention of ovarian cancer. Med J Aust. 2024 Mar 18;220(5):264-274. doi: 10.5694/mja2.52227. Epub 2024 Feb 14. PMID: 38353066; PMCID: PMC7617385.
- Webb PM, Jordan SJ. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017 May;41:3-14. doi: 10.1016/j.bpobgyn.2016.08.006. Epub 2016 Oct 3. PMID: 27743768.
- Ali AT, Al-Ani O, Al-Ani F. Epidemiology and risk factors for ovarian cancer. Prz Menopauzalny. 2023 Jun;22(2):93-104. doi: 10.5114/pm.2023.128661. Epub 2023 Jun 14. PMID: 37674925; PMCID: PMC10477765.
- Whelan E, Kalliala I, Semertzidou A, Raglan O, Bowden S, Kechagias K, Markozannes G, Cividini S, McNeish I, Marchesi J, MacIntyre D, Bennett P, Tsilidis K, Kyrgiou M. Risk Factors for Ovarian Cancer: An Umbrella Review of the Literature. Cancers (Basel). 2022 May 30;14(11):2708. doi: 10.3390/cancers14112708. PMID: 35681688; PMCID: PMC9179274.
- Khanlarkhani N, Azizi E, Amidi F, Khodarahmian M, Salehi E, Pazhohan A, Farhood B, Mortezae K, Goradel NH, Nashtaei MS. Metabolic risk factors of ovarian cancer: a review. JBRA Assist Reprod. 2022 Apr 17;26(2):335-347. doi: 10.5935/1518-0557.20210067. PMID: 34751020; PMCID: PMC9118962.
- Saso S, Barcroft JF, Kasaven LS, Galazis N, Ní Dhonnabháin B, Grewal KJ, Bracewell-Milnes T, Jones BP, Getreu N, Chan M, Mitra A, Al-Memar M, Ben-Nagi J, Smith JR, Yazbek J, Timmerman D, Bourne T, Ghaem-Maghami S, Verbakel JY. An umbrella review of meta-analyses regarding the incidence of female-specific malignancies after fertility treatment. Fertil Steril. 2025 Mar;123(3):506-519. doi: 10.1016/j.fertnstert.2024.09.023. Epub 2024 Nov 14. PMID: 39545878.
- Tanha K, Mottaghi A, Nojomi M, Moradi M, Rajabzadeh R, Lotfi S, Janani L. Investigation on factors associated with ovarian cancer: an umbrella review of systematic review and meta-analyses. J Ovarian Res. 2021 Nov 11;14(1):153. doi: 10.1186/s13048-021-00911-z. PMID: 34758846; PMCID: PMC8582179.
- Tanha K, Mottaghi A, Nojomi M, Moradi M, Rajabzadeh R, Lotfi S, Janani L. Investigation on factors associated with ovarian cancer: an umbrella review of systematic review and meta-analyses. J Ovarian Res. 2021 Nov 11;14(1):153. doi: 10.1186/s13048-021-00911-z. PMID: 34758846; PMCID: PMC8582179.